Yellow fever: The next big climate change-induced health threat?
Global health experts expect a drastic rise in yellow fever cases as the disease spreads to new areas in the coming years, fueled in part by climate change. Can innovation help halt its spread?

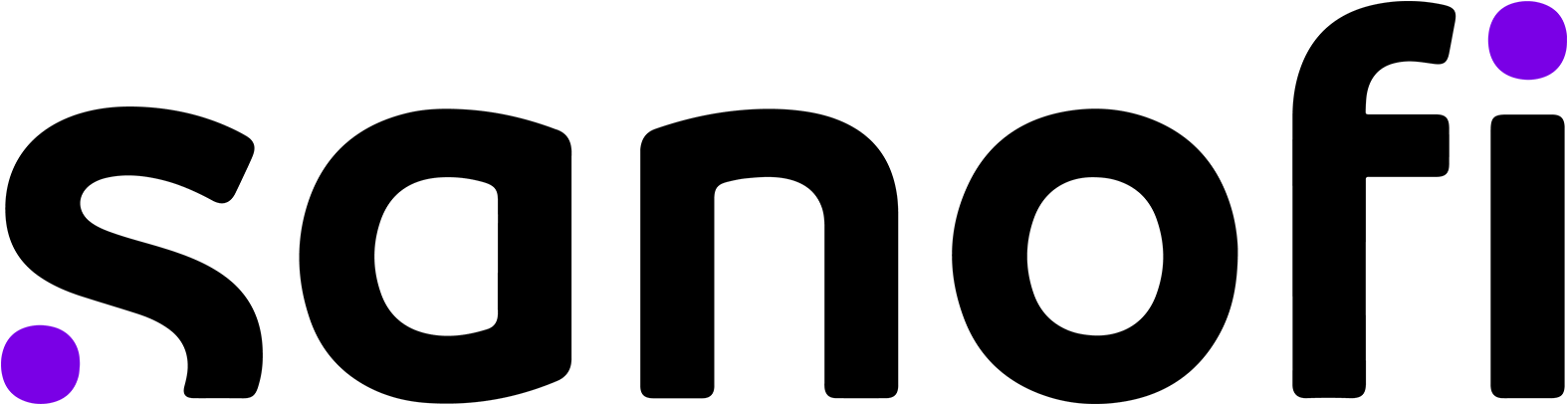
Long before COVID-19, a strange disease swept across the planet. Symptoms included fever and nausea, but in extreme cases, victims began to hemorrhage or bleed from the eyes, nose, and mouth.
In some regions of the world, the dreaded disease became known as “black vomit.” Jaundice and yellowing of the eyes would give it a more popular name: yellow fever.
André Mazet tending people suffering from yellow fever in the streets of Barcelona. Lithograph by Langlumé after J. Arago. Source: Wellcome Collection, Public Domain Mark
André Mazet tending people suffering from yellow fever in the streets of Barcelona. Lithograph by Langlumé after J. Arago. Source: Wellcome Collection, Public Domain Mark
Carried by primates — both human and nonhuman — and transmitted by the bites of infected mosquitoes — mainly from Aedes and Haemagogus species — yellow fever has wreaked havoc for nearly 3,000 years.
Scientists believe that it originated in Africa, spreading to the Americas in the 15th and 16th centuries on slave ships and barges by mosquitoes living in water barrels.
Once it arrived, the disease decimated armies and killed thousands of people from Bermuda to Philadelphia.
For centuries, scientists scrambled to tackle the deadly disease with no cure. Then in the 1930s, a vaccine was developed. It proved to be highly effective.

A scientist wearing a face mask works at a laboratory bench with bunsen burners and microscopes. Photograph, 1910/1930 (?). Source: Wellcome Collection, Public Domain Mark
A scientist wearing a face mask works at a laboratory bench with bunsen burners and microscopes. Photograph, 1910/1930 (?). Source: Wellcome Collection, Public Domain Mark
Along with mosquito control measures, vaccination helped to pause yellow fever’s reign of terror and is now regarded as being the most important means to help prevent outbreaks. At least 80% of the at-risk population need to be vaccinated to help prevent transmission.
In the past six years, explosive outbreaks have seen yellow fever re-emerge as a major international public health threat in endemic areas, fueled by insufficient vaccination coverage, as well as climate factors, population growth, and urbanization.
The resurgence of this deadly disease — approximately half of the small proportion of yellow fever patients who develop severe symptoms die within 7 to 10 days — cannot be ignored, especially in the face of expanding conditions for its spread.
Climate change is amplifying mosquito-borne diseases
Currently, the yellow fever virus is estimated to cause an estimated 109,000 severe cases of disease and 51,000 deaths each year, with 90% occurring in Africa. Despite spending millions of dollars each year in attempting to decrease mosquito populations and launching public awareness campaigns, countries across Africa and Latin America are continuing to report increases in mosquito populations and yellow fever cases.
In the next 30 years, nearly half a billion more people could be at risk for contracting mosquito-borne diseases like yellow fever, dengue, chikungunya, and Zika — all of which are transmitted by the same type of mosquito.
Climate change is considered to be “one of the main drivers of the ecology of these mosquitoes,” said Felipe Colón-González, the technology lead in the data for science and health team at the Wellcome. Increased resistance of mosquitoes to traditional insecticides is also likely to be an aggravating factor in the future.
“In general, warmer temperatures help the mosquitoes develop and reproduce faster, leading to more mosquitoes and therefore a higher risk of people getting infected. Rainfall can also increase mosquito abundance, as it generates breeding sites for them to lay eggs in,” explained Colón-González.
As a result, the yellow fever virus could be introduced to large urban populations that have not been vaccinated or previously exposed to the disease. This could have dramatic consequences. Modeling from Imperial College London shows that yellow fever deaths across Africa could increase by up to 25% by 2050 in the worst-case scenario. Additionally, one study showed that the Aedes aegypti mosquito could reach new temperate areas in the United States and China as far north as Chicago and Shanghai by 2050.

Impact of environmental changes and mass displacement on the threat of yellow fever
It’s not just hotter weather but another environmental issue — deforestation — that could exacerbate the threat. “Deforestation makes it more likely that humans will be in forests to work or live closer to forest areas where nonhuman primates live who carry yellow fever virus, and therefore the mosquitoes in that area are more likely to transfer it to them,” explained Katy Gaythorpe, the author of the study from Imperial College and the lead researcher for the Vaccine Impact Modelling Consortium. Nonvaccinated people bitten by infected mosquitoes might then return to a more densely populated area and spread the disease, especially in areas with large mosquito populations and an insufficient vaccination coverage rate.
In addition, extreme weather events are also causing social changes that come with disease risks: driving mass displacement, causing thousands of climate refugees worldwide to relocate from rural communities to major cities.
Cassandra Quintanilla, senior manager for vaccine programs at Gavi, outlines the impacts of climate change on global health.
“We've seen yellow fever go into regions where we haven't seen it before or where we thought we had tackled it before,” said Cassandra Quintanilla, senior manager for vaccine programs at Gavi, the Vaccine Alliance. Quintanilla cited the 2021 outbreaks that affected West and Central Africa as an example.
“In some of these countries, we've had mass vaccination campaigns in the past, and so we would assume that there was a big area already protected.” Population movements, decreasing vaccine coverage rates, and stress on health systems due to the COVID-19 pandemic and other public health crises are all factors that likely contributed to this resurgence. Up until late 2020, there had been minimal numbers of yellow fever cases detected in the region.
Various hard-to-predict variables, such as the impact of extreme-hot temperatures on mosquitoes or the effects of deforestation on the population of nonhuman primates, make the picture by 2050 not entirely clear-cut, Gaythorpe suggested. But despite these variables, there is a consensus among experts that changes in weather and migration patterns will contribute to a higher burden of yellow fever.

Yellow fever is transmitted and spread to humans in three ways
Source: World Health Organization
Sylvatic (or jungle) yellow fever:
In tropical rainforests, nonhuman primates such as monkeys are the primary reservoir of yellow fever. They are bitten by wild mosquitoes, which pass the virus on to other primates. Humans working or traveling through the forest may be bitten by infected mosquitoes and develop yellow fever.
Intermediate yellow fever:
In this type of transmission, semi-domestic mosquitoes — those that breed both in the wild and around households — infect both monkeys and people. Increased contact between people and infected mosquitoes leads to increased transmission and many separate villages in an area can develop outbreaks at the same time. This is the most common type of outbreak in Africa.
Urban yellow fever:
Large epidemics occur when infected people introduce the virus into heavily populated areas with high density of Aedes aegypti mosquitoes — which can breed in urban environments such as water containers — and where most people have little or no immunity, due to lack of vaccination or prior exposure to yellow fever. In these conditions, infected mosquitoes transmit the virus from person to person.
New strategies and long-term vaccine forecasting needed
There are several strategies needed to bolster the response and get prepared to address the expected rising risk of yellow fever.
Vaccination is “a no-brainer,” according to Quintanilla. One dose provides long-lived protection against the disease for most people. “So really it can be one of the most successful tools,” she added.
Other important interventions include wider surveillance of vectors, mosquito control activities, and investment in early warning systems, particularly in potential hot-spot areas, said Colón-González.
The development of technologies that incorporate climate information into early warning systems for infectious diseases is another important step, according to Colón-González, who said that work in this field is “gradually progressing and showing potential.” Reliable long-term forecasts are crucial to securing necessary vaccine supply for at-risk populations. However, integration of climate information in yellow fever vaccine long-term demand forecasts is still not a reality.
A key part of forecasting is commitment to a long-term sustainable vaccination program that instills confidence in manufacturers regarding vaccine demand, said Dr. Kate O’Brien, WHO’s top vaccines expert, during a podcast with the Eliminate Yellow Fever Epidemics strategy team. The EYE strategy was developed by a coalition of partners, including the World Health Organization and Gavi, the Vaccine Alliance after the 2016 outbreaks in Angola and the Democratic Republic of Congo.
The balance between vaccine demand and supply is very fragile, explained Lamia Badarous, head of public affairs for endemic vaccines at Sanofi. According to Badarous, underestimating the need in the face of rising risk would certainly be a problem, but oversupplying the market would also negatively impact the sustainability and viability of manufacturing. Market saturation and entry of multiple new suppliers will provide the wrong signal to existing manufacturers, leading them to scale down production or even exit the market, potentially jeopardizing the security of global supply and limiting access to innovation. To avoid this, accurate long-term forecasting and good coordination between global health partners and industry are needed.
Strong partnerships and innovation are essential to prepare for the future
Although vaccines have been available for almost a century, lack of access continues to be a challenge in some high-risk areas. Cross-sector commitment — from global institutions, governments, and industry — to increasing vaccination coverage rates is needed. Gavi, for example, is working with UNICEF and other EYE strategy partners on bringing yellow fever vaccination to high-risk regions that lack routine coverage. “We are focusing most of all on those pockets of populations that … not only don't have the yellow fever vaccine but also maybe don't have any other vaccine,” Quintanilla said.
In addition to improved vaccination coverage, early detection is critical to ensure the most effective response to outbreaks. “While yellow fever often has serious symptoms and has a high mortality rate for those infected, it can also be mild, or people may be asymptomatic,” Gaythorpe said. Innovation to improve diagnosis and surveillance is therefore a key priority area. Gavi is supporting countries with laboratory capacity strengthening to enable them to detect where cases are happening and access the stockpile faster, as well as give them a better understanding of how they can use the vaccine in a preventive way, explained Quintanilla.
Innovation is also essential for vaccines. “All current manufacturers are working with an egg-based technology. We need to encourage innovation so that new vaccines are more easily developed and delivered rapidly to the populations in need,” Badarous said.

Copyright: Sanofi / Patrick Boulen
Copyright: Sanofi / Patrick Boulen
The 2016 outbreak in Angola and DRC exposed glaring weaknesses in the emergency vaccine supply pipeline. Despite a global stockpile of six million doses that is regularly replenished, nearly five times more doses were needed to end the outbreak. Ultimately, public health experts opted to give fractional doses to prolong supplies.
According to Badarous, this was a valuable lesson for the global health community. “What we’ve really learned is that we need to be ready and to anticipate future large, unexpected outbreaks, especially in the context of climate change, as part of epidemic preparedness,” she said. Development of new yellow-fever vaccines that can be produced in a shorter timeframe and have the potential for higher production yields is critical for securing stockpiles and emergency response.
Ultimately, Badarous said that any vaccine innovation needs to have the united backing of the global health community, along with long-term demand forecasts incentivizing manufacturers to sustain investments. “For innovation to survive it needs to be incentivized by all actors from the global health ecosystem. That can really be a game changer.”
SPONSORED BY
MAT-GLB-2301187
Visit the Planet Health series for more in-depth reporting on the current impact of the climate crisis on human health around the world. Join the conversation by using the hashtag #PlanetHealth.