The neglected of the neglected: tackling noma
Noma affects thousands each year yet research and resources for it are limited. In northwestern Nigeria, one hospital is dedicated to fighting it.

In the Noma Children Hospital in Sokoto, in northwestern Nigeria, Mulikat Okanlawon, a hygiene officer, spends her days caring for patients. Many are recovering from reconstructive facial surgery, others are waiting, hoping that their being there marks the start of their road to recovery from a devastating disease.

Noma Children Hospital in Sokoto, northwest Nigeria, is the only hospital in the country dedicated to this neglected and devastating infection. It provides free medical care, including reconstructive surgery, for people affected by noma. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Noma Children Hospital in Sokoto, northwest Nigeria, is the only hospital in the country dedicated to this neglected and devastating infection. It provides free medical care, including reconstructive surgery, for people affected by noma. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Noma is a facial gangrene infection that attacks facial tissue and bone before killing around 90% of its victims within a few weeks. Although data is scarce, it’s estimated that the annual global incidence sits between 30,000 and 40,000, the majority of which are in sub-Saharan Africa and in children between the ages of 2 and 6.
Malnutrition, extreme poverty, and poor access to WASH create prime conditions for noma, meaning people from lower-income and remote communities are disproportionately affected.
Stages of development of noma.
Stages of development of noma.
Those lucky enough to reach a health care facility and receive a correct diagnosis can be treated through wound dressing, improved hygiene and nutrition, and a combination of antibiotics. Yet often they are left with facial deformities that can cause life-long difficulties in eating, speaking, and breathing.
Okanlawon contracted noma at 6 years old and survived the initial infection. It would be almost 10 years before a stranger in the street would recognize her condition as noma. Having heard of the work being done in Sokoto, he recommended she travel there from her home in Lagos. “He told me that by the time they operated on me I would like myself,” she said.
In 1999, Okanlawon was among the hospital’s first surgical patients.
A lack of research makes the prevalence hard to determine

In Nigeria, between 2010-2018 the national incidence of noma was noted at between 4.1 to 17.9 per 100,0000 people. Cases have been frequently reported in other countries in the Sahel as well as in Laos and Haiti. But few studies are available on noma’s prevalence and the figures that are available are likely underestimates, Kamran Rafiq, co-founder and communications director of The International Society for Neglected Tropical Diseases, said.

Yaashe, a 6-year-old noma patient from Borno state. She received surgery six months after arriving at the Noma Children Hospital. It’s the first of several operations she needs because of the severity of her injuries. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Yaashe, a 6-year-old noma patient from Borno state. She received surgery six months after arriving at the Noma Children Hospital. It’s the first of several operations she needs because of the severity of her injuries. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
The rapid progression and high-mortality rate combined with beliefs that such an ailment could be a divine punishment, preventing families from seeking treatment, affects what’s known about noma’s prevalence.
Awareness raising can help.
In January 2017, the outreach team at the Noma Children Hospital of Sokoto started working to find active cases in the Sokoto state. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
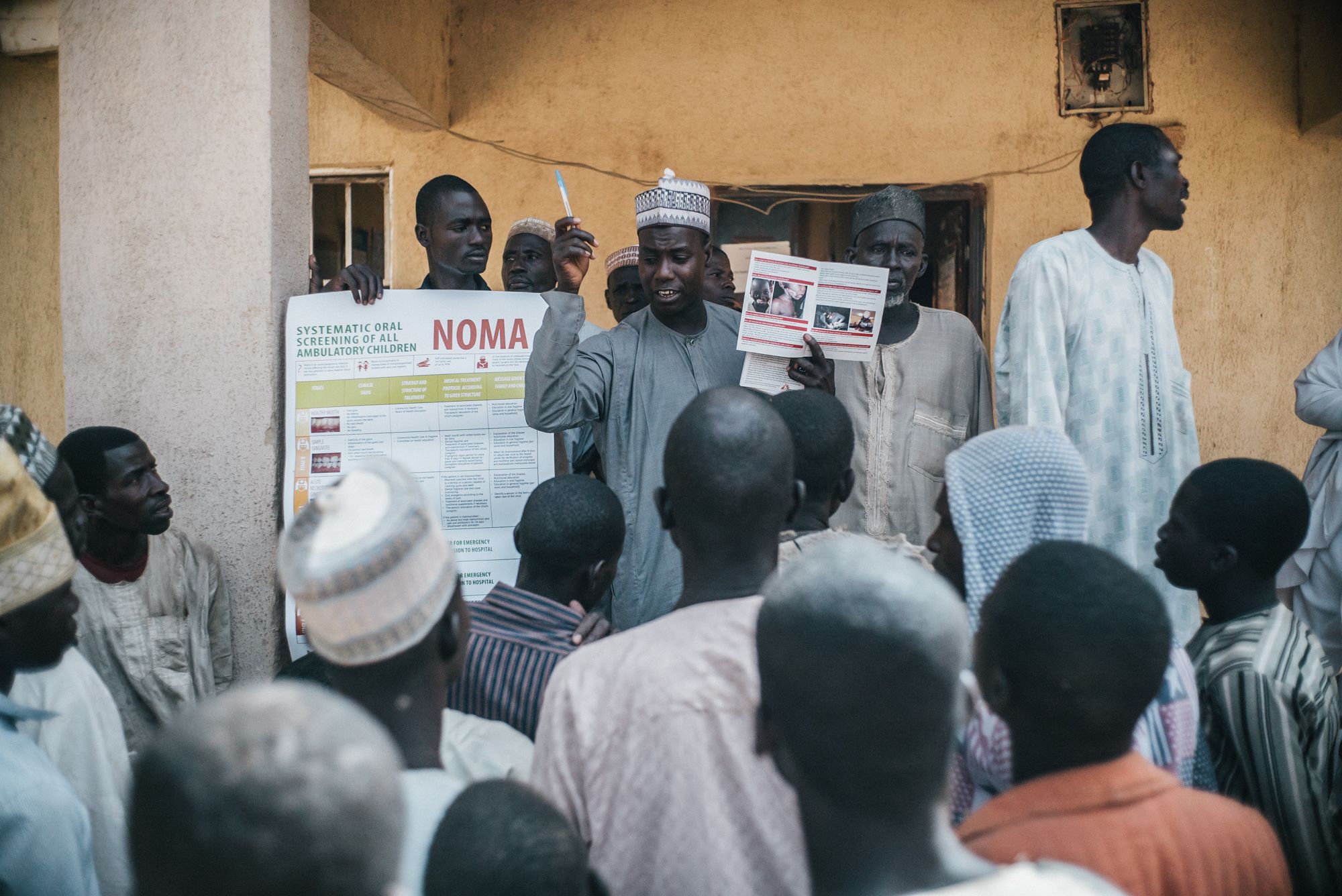
Leaflets are used to help identify potential noma patients. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz

The team also informs people about the causes of noma and the need to be treated in the early stages. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz

Okanlawon, in her role as a hygiene officer at Médecins Sans Frontières, said she sees 10 fresh cases of noma per month on average at the Noma Children Hospital, which is run by the Ministry of Health and has been supported by MSF since 2014. The 92-bed hospital is the only one dedicated to noma in Nigeria. The reason she sees so many is in part because of the hospital’s outreach team, she said, which disseminates prevention messaging and conducts active case finding.

Adebowale Murtala, MSF counsellor educator in Noma Children Hospital, visits the postoperative ward every day to check how patients are dealing with the painful recovery from the reconstructive surgery. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Adebowale Murtala, MSF counsellor educator in Noma Children Hospital, visits the postoperative ward every day to check how patients are dealing with the painful recovery from the reconstructive surgery. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
“We try to make everyone, including health providers, know what noma is, how it presents and starts and what should someone do if they see a patient with noma,” explained Dr. Isah Shafiu, chairman of the medical advisory committee at the hospital. Any patients diagnosed by the outreach team or other in-country MSF factions are referred to Sokoto for free care.
If the patient doesn’t want to travel, antibiotics and nutrition treatment are provided in the hope that they’ll consider coming for a reconstructive surgery at a later date, Dr. Bukola Oluyide, deputy medical coordinator at MSF in Nigeria, said.
At the hospital, more testing and treatment for any comorbidities — including sepsis, dehydration, and malnutrition — takes place before there’s an assessment for reconstructive surgery. When overseas surgical teams who visit quarterly arrive, usually around 30 patients await a procedure. Oftentimes multiple surgeries and physiotherapy is needed across several years.
In 2019, teams performed 178 surgeries on 129 patients. In 2020, surgeries were more than halved as a result of COVID-19, but have since resumed with in-country surgeons taking the lead.

Four times a year, a team of highly trained plastic and maxillofacial surgeons, anesthesiologists, and nurses from all over the world arrive at Sokoto's Noma Children Hospital to perform reconstructive surgery for noma patients. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Four times a year, a team of highly trained plastic and maxillofacial surgeons, anesthesiologists, and nurses from all over the world arrive at Sokoto's Noma Children Hospital to perform reconstructive surgery for noma patients. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Okanlawon explained that surgery helps to tackle the stigma surrounding facial disfigurement; she herself has undergone several operations. “Nobody wanted to see me before the operation … If I was coming, they’d all run,” she said. But post-op, that all changed. “I’m a new person now. I’m a new Mulikat,” she said, adding that these days people are happy to see her.
Following her surgery, the hospital hired Okanlawon to share her experiences as part of pre- and post-surgery psychosocial support. “Any patients who see me will know when there is life there is hope,” she said.
While efforts like that of Okanlawon and Sokoto’s Noma Children Hospital are a good example of the work being done to prevent and treat noma, such examples are rare. The fact that many have never heard of noma means attention, funding, and resources are limited.

Facial plastic and reconstructive surgeon David Shaye examines Hadiza, a 40-year-old patient from Kano State, during a screening session at the Noma Children Hospital in Sokoto, Nigeria. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Facial plastic and reconstructive surgeon David Shaye examines Hadiza, a 40-year-old patient from Kano State, during a screening session at the Noma Children Hospital in Sokoto, Nigeria. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Noma as an NTD

At February's noma conference, many called for the World Health Organization to recognize noma as a neglected tropical disease in its 2023 review process.
While included in the PLOS Medicine NTD list and targeted in WHO’s Africa regional program and WHO’s Oral Health Program, it’s thought noma’s adoption to WHO’s NTD list — of which 20 diseases are listed — would mean increased resources.
“From an advocacy perspective, it’d be awesome to be on that list,” Rafiq said, and from a finance perspective, it could trigger a funding cascade for research. “The mad thing about noma is this is a totally preventable disease so can you imagine the win-win scenario at the end if someone was trying to get involved in this from a financial perspective,” Rafiq said.
"There's a paradox: no funds, no epidemiology. No epidemiology, no funds."
To qualify, a disease must disproportionately cause stigma, morbidity, and mortality among impoverished populations; primarily be found in tropical and sub-tropical areas, be amenable to control, elimination, or eradication through one of five public health strategies; and have limited research available. Multiple WHO member states must submit a request for inclusion with a dossier of supporting evidence.
The evidence poses a barrier for noma.

Bilya, a 20-year-old noma patient from a village near the border with Niger, talks with Samuel Joseph, a specialist nurse, the day before going to into surgery for the first time. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Bilya, a 20-year-old noma patient from a village near the border with Niger, talks with Samuel Joseph, a specialist nurse, the day before going to into surgery for the first time. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz




Sufyanu, a 3-year-old noma patient from Sokoto state, returned home with his parents and siblings after being treated in the Noma Children Hospital. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Sufyanu, a 3-year-old noma patient from Sokoto state, returned home with his parents and siblings after being treated in the Noma Children Hospital. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz

Mulikat, a former noma patient is pictured at the Noma Children Hospital where she has lived for 17 years. After graduating at 33 years old, she started working as a hygiene officer. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Mulikat, a former noma patient is pictured at the Noma Children Hospital where she has lived for 17 years. After graduating at 33 years old, she started working as a hygiene officer. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz

Adamu, a 14-year-old noma patient from Kebbi state, has a screening session at Noma Children Hospital in Sokoto. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Adamu, a 14-year-old noma patient from Kebbi state, has a screening session at Noma Children Hospital in Sokoto. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz

Amina, a 19-year-old noma patient from Yobe state, waits for the screening session at Noma Children Hospital in Sokoto. Amina came several times since her first visit in November 2016. This time, she travelled with her elder sister because her mother couldn't leave their area, being the beneficiary of the food distribution card for the whole family. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Amina, a 19-year-old noma patient from Yobe state, waits for the screening session at Noma Children Hospital in Sokoto. Amina came several times since her first visit in November 2016. This time, she travelled with her elder sister because her mother couldn't leave their area, being the beneficiary of the food distribution card for the whole family. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz

Hadiza, a 40-year-old patient from Kano state, smiles before getting her fourth reconstructive surgery. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Hadiza, a 40-year-old patient from Kano state, smiles before getting her fourth reconstructive surgery. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
A lack of high-quality and comprehensive research and “substantial gaps in knowledge” may hinder and delay the development and submission of a dossier, Dr. Yuka Makino, technical officer of oral health at WHO’s regional office for Africa, told Devex. She suggested the noma community prioritize documentation of its burden, and the delineation of effective strategies and interventions before 2023.
According to experts — who, in 2019, ahead of the WHO’s consultation process for the launch of the new NTD roadmap, asked for the assessment of progress on noma — this is “problematic.”
“If a disease is so neglected that it receives limited funding and consequently little research is conducted, how can evidence be provided to prove that it is neglected?” they asked. “There’s a paradox: no funds, no epidemiology. No epidemiology, no funds,” Rafiq said. “It’s about making that case.” In order to do that, more funding is required and more funding comes through increased awareness.
“If a disease is so neglected that it receives limited funding and consequently little research is conducted, how can evidence be provided to prove that it is neglected?”
Beyond the NTD nomenclature

While increased research should be a priority, interviewees agreed that being on the NTD list wouldn’t be the silver bullet anyway.
For Oluyide, the NTD recognition is a long-term ambition and there are things that can be done in the meantime.
“Policies that ensure food security is high, health facilities are available, nutritional services are available even at the grassroots level, and then awareness for people to come to these services would go a very long way in ensuring children don’t develop noma at all,” she said. This is even more paramount given the strain on resources posed by COVID-19 as well as the ongoing violence and insecurity exacerbating basic needs in the north of Nigeria.
Including noma in the training curriculum for health workers would also enable them to conduct screenings in local facilities and treat noma at an earlier stage, Oluyide said.
For Rafiq, the game changer will be in bringing different expertise to look at noma through perspectives such as WASH, technology, and other related health issues. This could offer some more solutions, he said.
Okanlawon called for continued financial support for the hospital and for the international community to continue raising awareness of noma. “I want them to put more effort into supporting us,” she said.




Aliyu, a 27-year-old noma patient, stands next to his home, in a village in Sokoto state. Aliyu says he usually covers his face with a veil to protect his wound from the sun or dust when he takes care of his cattle, but also due to shyness and discrimination he has faced in the past. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Aliyu, a 27-year-old noma patient, stands next to his home, in a village in Sokoto state. Aliyu says he usually covers his face with a veil to protect his wound from the sun or dust when he takes care of his cattle, but also due to shyness and discrimination he has faced in the past. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz

Maryam, aged 4, plays in the courtyard of the Noma Children Hospital. She has already undergone four reconstructive operations, including a skin graft taken from her chest to replace tissue destroyed by noma. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Maryam, aged 4, plays in the courtyard of the Noma Children Hospital. She has already undergone four reconstructive operations, including a skin graft taken from her chest to replace tissue destroyed by noma. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz

An outreach team of the Noma Children Hospital of Sokoto, Nigeria, is visiting a village in the local government of Gwadabawa. Active case finding is a key challenge as noma patients are usually living in remote villages, with no access to healthcare. Here, the team is showing leaflets to check if people can spot a potential patient in the area. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
An outreach team of the Noma Children Hospital of Sokoto, Nigeria, is visiting a village in the local government of Gwadabawa. Active case finding is a key challenge as noma patients are usually living in remote villages, with no access to healthcare. Here, the team is showing leaflets to check if people can spot a potential patient in the area. Photo by: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Photos/captions: Claire Jeantet / Fabrice Catérini / Chloe Fournier / Inediz
Production: Janelle Cruz
