How innovations in TB detection are transforming pediatric care in Bangladesh
To tackle stubbornly high rates of tuberculosis in children, government and nonprofit groups in Bangladesh are implementing a range of innovations including mobile X-ray machines with artificial intelligence, new molecular diagnostics, and better point-of-care service.

Rukaya, three and a half years old, hadn't been feeling well for the last couple of months. She had a stubborn fever that didn’t improve after taking medicine prescribed by her doctor, and her high temperature had been back for the last 15 days, explained her father, Gulzar Hossain.

Rukaya Hossain and her father, Gulzar, at Narsingdi Sadar Hospital, Bangladesh.
Rukaya Hossain and her father, Gulzar, at Narsingdi Sadar Hospital, Bangladesh.
“It was strange but I wasn’t too concerned,” he told Devex as a health worker took Rukaya’s medical history in the Integrated Management of Childhood Illness corner in Narsingdi Sadar Hospital, about 40 kilometers (29 miles) outside Dhaka, Bangladesh.


Integrated Management of Childhood Illness
Integrated Management of Childhood Illness, or IMCI, is a systematic approach to children's health developed by the United Nations in the 1990s. It encourages a holistic approach to pediatric care, as opposed to focusing on single diseases like malaria or measles, and an IMCI corner is often the first stop for sick children under five in developing countries.
The IMCI health worker believed Rukaya could be at risk for tuberculosis, a disease that killed an estimated 139,000 children under five worldwide in 2022. The results from a Tuberculin skin test, or TST, indicated that indeed she was a presumptive tuberculosis patient.
“I didn’t think it could have been tuberculosis. I’ve never had experience with it,” said Farida Parvin, Rukaya’s mother, before whisking Rukaya off to receive a chest X-ray. “But I feel relieved to be here and have the tests done. If it’s tuberculosis, we’ll follow the procedure.”
What appeared to be a routine intervention that caught a potentially deadly disease may not have taken place just a few years ago, when IMCI staff weren’t trained to see Rukaya’s history and symptoms as indicative of a possible tuberculosis diagnosis.


But in recent years, there’s been a major push to train IMCI staff members in identifying potential TB cases, led by national health authorities alongside local and international organizations including the International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b), the Stop TB Partnership, and The Global Fund to Fight AIDS, Tuberculosis and Malaria.
This, coupled with the deployment of a plethora of innovative diagnostic and treatment tools such as mobile X-ray units installed with artificial intelligence software, has resulted in significant gains in the fight to stop TB in high-burden countries such as Bangladesh.
The challenge of TB in children

Tuberculosis continues to be one of the leading causes of death by infectious diseases worldwide, killing 1.3 million people in 2022, according to the World Health Organization — more than HIV/AIDS and malaria combined.
Almost 10% of TB mortalities were in children, but there are significant challenges in diagnosing and treating the youngest patients: They carry lower viral loads, can’t produce sputum, which is vital for high-quality diagnostics, and their symptoms aren’t as obvious as those of adults. That’s why of the some 130,000 people whose TB infection was missed in Bangladesh in 2020, 15% were children.
Bangladesh has embraced a number of innovations for diagnosing and treating TB in children, explains Stop TB Partnership Executive Director Lucica Ditiu.
Despite these challenges, there is a belief among public officials and TB experts that the country has all the right tools to make significant progress in the fight against the disease.
“Bangladesh has an appetite [for innovation] in the public and private sector,” said Dr. Lucica Ditiu, executive director of the Stop TB Partnership. Organizations such as BRAC and icddr,b “are really frontrunners globally in embracing innovation,” she added.
Better diagnostics with AI-powered mobile X-rays

One of the biggest obstacles to stopping TB in low-income countries such as Bangladesh is the lack of high-quality diagnostics in underserved areas. Mobile X-ray units that can be transported in a backpack and set up with minimal staff are part of a new breed of innovation that could help overcome that access barrier.
Abdul Aziz, a rickshaw puller from Korial Basti, Dhaka’s largest slum, has had a cough for three months and a fever for the last five nights. The illness is affecting his ability to work, so when he heard from a community health worker that there would be a mobile X-ray unit at the local primary school, he made sure to come by.

After taking an X-ray of Aziz’s chest, medical technologists Sajal Roy and Nazmul Hasan process the image through the AI-powered software CAD4TB on their laptops. The software analyzes the condition of the patient’s lungs and provides a score out of 100, indicating the probability of an active tuberculosis infection. No more than 60 seconds after taking the X-ray, Aziz receives his score — it’s high and he’s instructed to provide a sputum sample that will confirm a TB diagnosis.

Rickshaw puller Abdul Aziz has had TB symptoms for several months, affecting his ability to work.
“This is just the beginning,” said Dr. Senjuti Kabir, assistant scientist at icddr,b’s emerging infections program, referring to the use of mobile AI-powered X-ray. Implemented by Bangladesh’s national TB control program in partnership with icddr,b and the Stop TB Partnership, the intervention will be scaled up in the coming months with a procurement of 40 new units.

Rickshaw puller Abdul Aziz has had TB symptoms for several months, affecting his ability to work.
Rickshaw puller Abdul Aziz has had TB symptoms for several months, affecting his ability to work.

A patient has an X-ray taken at a local primary school in Korial Basti, Dhaka's largest slum.
A patient has an X-ray taken at a local primary school in Korial Basti, Dhaka's largest slum.

In the coming months, the government will scale up the use of mobile X-ray with a procurement of 40 new units.
In the coming months, the government will scale up the use of mobile X-ray with a procurement of 40 new units.
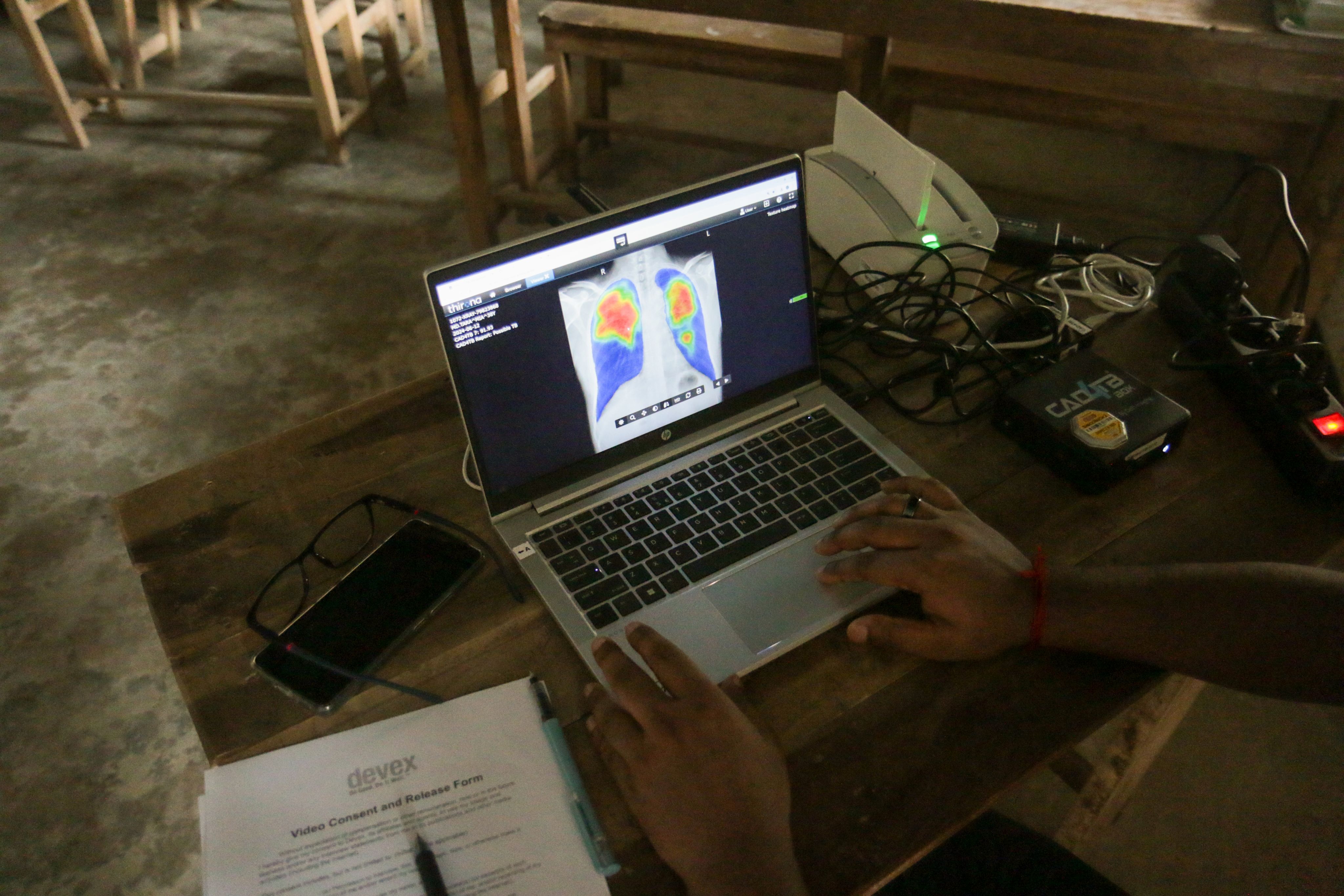
The image is processed using AI-powered software, which analyzes the condition of the patient's lungs.
The image is processed using AI-powered software, which analyzes the condition of the patient's lungs.
Pioneering molecular diagnostic tests

While AI-assisted X-ray technology has only been approved by the World Health Organization for use in adults, many believe that the next logical innovation is trialing its use with children. Bangladesh has already been at the forefront of another diagnostic innovation that has significantly improved the detection of TB in children under five years old — the use of stool samples instead of sputum in molecular diagnostic tests like Xpert technology.
Before 2020, when WHO started recommending the use of stool for diagnosing TB in children, medical professionals had to rely on invasive methods such as nasogastric aspiration and sputum induction, which cause significant discomfort for children and require expertise that is lacking in many primary health care facilities.
Bangladesh helped pioneer research into TB diagnosis with stool samples and local stakeholders are now looking to further innovation in this arena.

A lab technician inserts sputum samples into a GeneXpert machine.
A lab technician inserts sputum samples into a GeneXpert machine.

Lab technicians analyzing sputum samples.
Lab technicians analyzing sputum samples.

Lab technicians prepare sputum samples for molecular diagnostics.
Lab technicians prepare sputum samples for molecular diagnostics.
Currently, WHO only recommends using stool samples in Xpert technology. The problem is that GeneXpert, a gold standard in TB diagnostics, requires a sophisticated, energy-intensive laboratory setting, limiting its use beyond hospitals, where the majority of missing cases need to be diagnosed. That’s where new innovations in molecular diagnostics like Truenat, a portable, real-time PCR testing technology for TB, come in.
Truenat resolves many of the issues around resource and cost intensity that come with Xpert technology, since it’s operated handheld and with batteries. The result is a highly accurate diagnostics test that can be used in patients’ homes. Bangladesh has been ramping up Truenat use through the Stop TB Partnership and the United States Agency for International Development’s introducing New Tools Project, or iNTP, which piloted a 2022 project with 38 Truenat Duo systems. The iNTP also plans to acquire another 112 through the Global Fund in the coming years.
But many feel that Truenat, like AI-assisted X-ray, isn’t currently being used to its full potential. As of now, insufficient research has been conducted utilizing stool samples with Truenat, which would open doors to diagnosing children under five who can’t access a hospital setting, said Ditiu.

As attractive, and useful, as advancements in diagnostic technology can be, often the most effective interventions can be simple changes in medical procedures. Under current national tuberculosis guidelines, a child would need to show symptoms such as more than two weeks of cough or two weeks of fever to be tested for TB. But children under five often present with nonspecific signs and symptoms, which is the main reason why almost 70% of tuberculosis cases among children under five are missed, according to WHO.
As part of a series of interventions called TB Reach Wave 10, Stop TB in partnership with icddr,b is piloting a change in pediatric care provided through IMCI corners that would significantly expand the symptoms or signs considered indicative of tuberculosis in children.
Instead of just a few weeks of cough and fever or weight loss, symptoms that qualify children like Rukaya to be tested for TB include any swollen lymph nodes, contact with a family member with TB, and diarrhea for more than two weeks, among others.
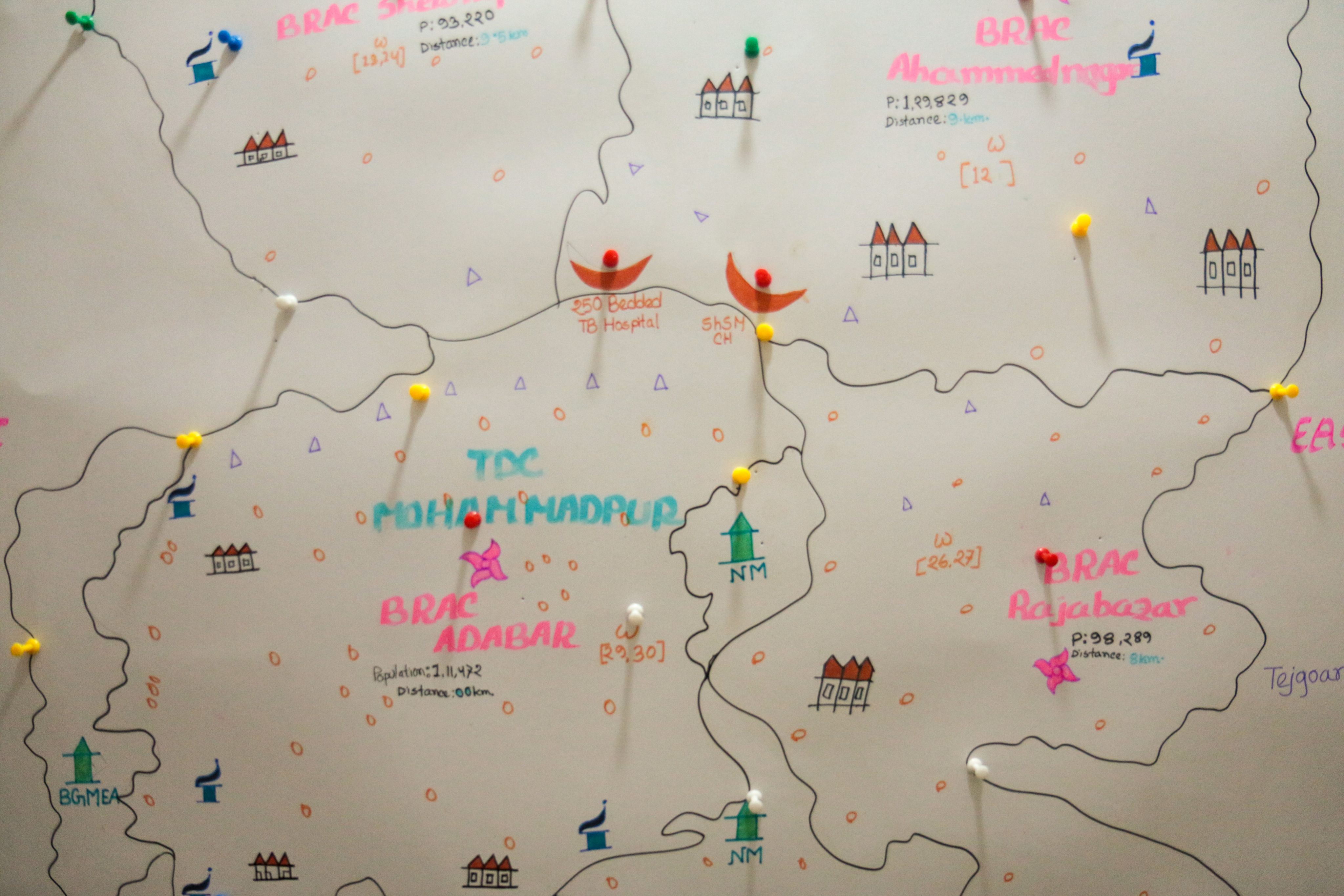
A map showing TB operations conducted by the nonprofit BRAC.
A map showing TB operations conducted by the nonprofit BRAC.

Jakia Khatun, a medical technologist with the BRAC health program.
Jakia Khatun, a medical technologist with the BRAC health program.
In addition to capacity building for IMCI providers, the project also includes developing an app-based tool for taking patient data and history and introduces robust contact investigation, which is crucial given that children under five almost always get TB from a family member.
“The diagnosis of TB is not very difficult,” said Dr. Tahmeed Ahmed, executive director of icddr,b. “The challenge is that not many health practitioners are aware of [diagnostic practices].”
Dr. Tahmeed Ahmed, executive director of icddr,b, gives an overview of the burden of adult and child TB in Bangladesh.
The initial results of the program are promising. The Narsingdi Sadar Hospital, where Rukaya was received, saw the number of children diagnosed with TB double in the period January to March, 2024 compared to the same period the prior year, before the project was implemented, according to data compiled by the hospital.
Hospital staff are noticing the change in workload. “I’m getting way more X-ray patients — five to seven per day, up from just a few,” said Rashida Parvin, an X-ray technologist at the hospital. “It’s more work but I’m happy because the children are getting evaluated.”
Incorporating TB screening into the IMCI corners has lifted a huge burden on pediatricians, who can see up to 150 children per day in local health centers in Narsingdi District, says Dr. Farhana Ahmed, civil surgeon of Narsingdi District. “This project gives us skilled manpower,” she said.
How climate change will impact the campaign against TB

While Bangladesh has seen significant success in fighting TB — it is one of just eight countries that have reduced mortalities from TB by 35% since 2015, according to WHO — its positive momentum could be complicated by a range of factors, in particular climate change.
With two-thirds of the country under 15 feet above sea level, Bangladesh is one of the most at-risk countries in the world when it comes to climate change. Extreme weather events will most likely exacerbate migration from coastal and rural areas to larger cities such as Dhaka, where a lack of infrastructure has led to a rapid expansion of informal housing.
The living conditions of migrants is a key element in the fight against TB. “TB as a pathogen likes nothing more than undernourished, stressed people living in very crowded circumstances,” Peter Sands, executive director of the Global Fund, told Devex.
Crucially, there needs to be a blurring of boundaries between nutrition and medicine to completely eradicate TB, especially in the face of climate change, said Sands. “What we find in climate change-affected settings is that populations are more vulnerable to illness and food shortages.”
With climate change’s impact on Bangladesh’s vulnerable population looming, partners believe it’s crucial not to lose focus on stopping TB in the country. And due to the nature of how children under five get TB (through adults), the levels of TB in the youngest age group is one of the best indicators of a country’s success in fighting the disease.
Update, Sept. 3, 2024: We’ve updated this story to clarify that the x-ray images are being processed using the AI software CAD4TB.

Reporting, video, and photos by Nathan Siegel
Edited by Naomi Mihara and Richard Jones
Video editing by Mai Ylagan
Shorthand production by Naomi Mihara
Produced in partnership with

Visit the Talking TB series for more coverage on how we can eliminate tuberculosis by 2030. The time for a paradigm shift and a renewed focus on funding, research, and global solutions is now. Join the conversation by using the hashtag #TalkingTB.


