How decentralized testing is advancing TB diagnosis and treatment
Delayed diagnosis is deadly for tuberculosis, which can take months to present and treat, but access to tools to bring diagnosis directly to communities is helping to save lives. Devex spoke to medics in three high-burden countries to find out more.

SPONSORED BY

For tuberculosis patients in Karamoja, a region in northeastern Uganda close to the Kenyan border, getting access to the full course of TB treatment required can be difficult. Long distances to health facilities and poor roads can mean many patients drop out of the system between initially seeking out care and actually getting the diagnosis needed to be prescribed medicine.
To address this, the local St. Kizito Matany Hospital has adopted various solutions to bring testing closer to communities. This is to help ensure patients get early diagnosis and treatment, which can last from nine months to 20 months for stubborn cases of drug-resistant TB, Dr. Faustine Erau, a clinical officer and TB coordinator at the hospital, told Devex. Without treatment, the death rate from TB is about 50%.
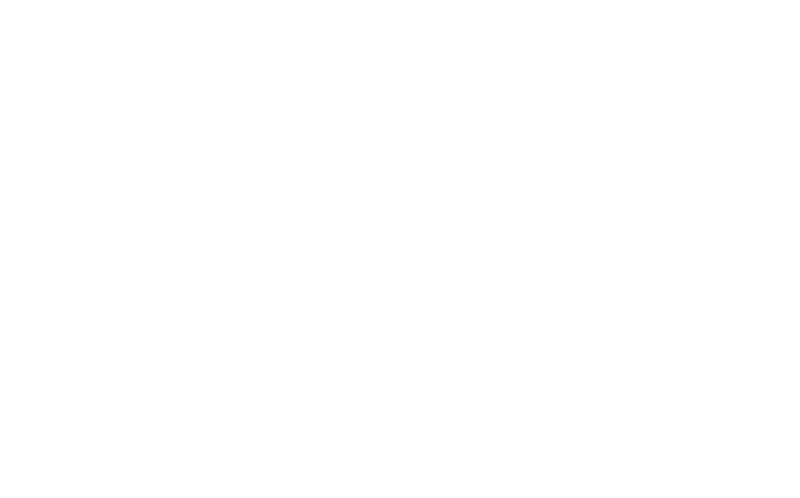
Laboratory assistant at St. Kizito Matany Hospital Laboratory in Karamoja, Uganda, reviewing data from TB diagnostic tests. Photo: Innocent Twebaze
Laboratory assistant at St. Kizito Matany Hospital Laboratory in Karamoja, Uganda, reviewing data from TB diagnostic tests. Photo: Innocent Twebaze
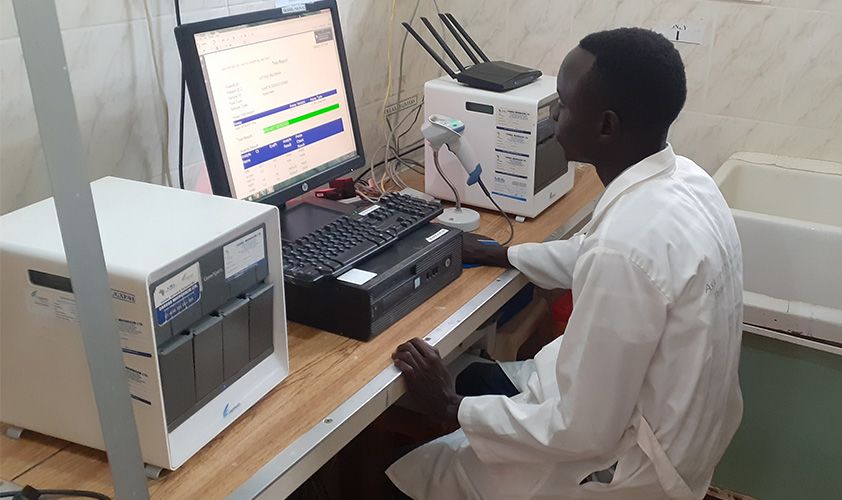
“We implemented a menu of community-based approaches, such as involving the village health teams, the community, linkage facilitators, and even expert clients to participate in the screening of patients in the community,” he said.
Former TB patients who have been cured are recruited as so-called expert clients to help with everything from educating communities to sample collection and delivery to diagnostic centers, Erau said.
While COVID-19 temporarily overtook TB as the deadliest infectious disease in the height of the pandemic, TB is once again the world's biggest infectious killer and claimed some 1.6 million lives in 2021, according to the World Health Organization. The same year, an estimated 10.6 million people fell ill with TB. However, low- and middle-income countries shoulder a disproportionate burden of the disease, accounting for over 80% of TB cases and deaths.

Ending the TB epidemic by 2030 is among the health targets of the United Nations Sustainable Development Goals, but $13 billion in financing is needed annually for TB prevention, diagnosis, treatment, and care to achieve the global target agreed at the 2018 UN high-level meeting on TB. The UN General Assembly held the second high-level meeting on the fight against TB on Sept. 22, 2023.

Progress on eliminating the treatable disease took a huge hit during the COVID-19 pandemic, as disruptions to health services and lockdowns drastically decreased the number of people diagnosed with TB. In Vietnam, for example, the number of TB patients detected in 2021 had decreased by 24.5% compared to 2019, making Vietnam one of the countries with the highest reduction in TB detections globally.
However, the pandemic also showed the world what can be achieved through the mobilization of political will, finance, and human resources, as the Global Plan to End TB 2023-2030 states. And without immediate concrete action, an estimated 28 million people will die from TB by 2030, at a global economic cost of USD $1 trillion.
Devex spoke to health practitioners in Uganda, Pakistan, and Vietnam to find out what it takes to successfully implement community-based TB testing programs.
Better, faster testing for communities in Uganda
Community-based and ambulatory care typically leads to better TB outcomes compared to hospital-based or inpatient care, and WHO guidelines recommend that TB care be provided mainly in community-based and ambulatory settings when possible. Yet, 4.2 million people were estimated to go undiagnosed or unreported to national authorities in 2021.
Before Erau joined the St. Kizito Matany Hospital six years ago, and acquired a GeneXpert® machine — a molecular diagnostic system that uses cartridges for rapid TB diagnosis — the hospital was mainly using microscopes to diagnose TB. “It had its own challenges … sometimes you had to wait for a week to get results. It wasn’t until we received the GeneXpert machines that we started having on-time results. In two-three hours, you have your results,” he said.
Dr. Faustine Erau, clinical officer and TB coordinator at St. Kizito Matany, explains how on-site testing has improved the patient experience by enabling early and more accurate diagnosis.
“USAID’s PACT Karamoja project has been instrumental in providing technical assistance to laboratory staff, managing GeneXpert cartridge supply and distribution, and supporting staff to process sputum samples in peak seasons and off-clinic hours,” Erau added.
Today, each of the region’s nine districts has a GeneXpert system, and each one is utilized a lot, according to Erau. But the high-burden regions still need more machines to meet the high demand for testing, as well as more x-ray machines, he said.

St. Kizito Matany Hospital team and staff from the Infectious Disease Institute review quarterly TB patient data from the community. Photo: Dr. Faustine Erau
St. Kizito Matany Hospital team and staff from the Infectious Disease Institute review quarterly TB patient data from the community. Photo: Dr. Faustine Erau
Earlier this year, WHO issued technical testing program guidance stating that WHO-recommended rapid diagnostics for TB diagnosis “should reach all primary health care facilities systematically and progressively.” While the goal is for all notified patients to be tested with a rapid diagnostic tool by 2025, only 38% of patients receive the test today, and access to diagnostics remains a critical issue.
In Karamoja, on-site testing has significantly improved the patient experience by enabling early and more accurate diagnosis. This in turn has led to quicker treatment and relief of symptoms and helps prevent more serious complications, ultimately improving the health outcomes of the patient, according to Erau.
“Just imagine someone who has been sick for a year and they have been making the wrong diagnosis. We have seen scenarios of people coming and the whole lung was eaten up by this disease,” he said.
Chest camps in Pakistan bring care to marginalized communities

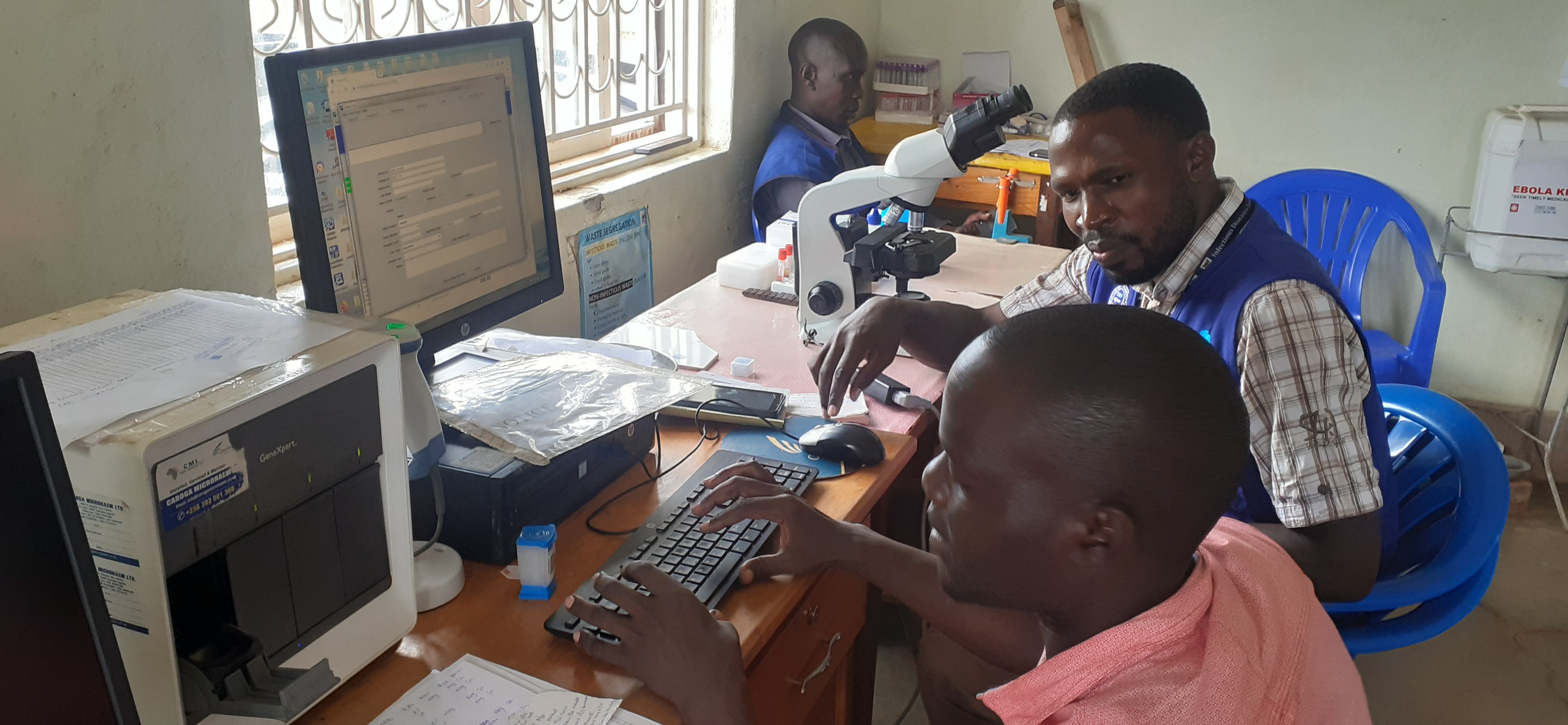
In Pakistan, the international humanitarian organization Mercy Corps is bringing TB testing closer to marginalized communities through mobile clinics known as chest camps. “TB is a disease of poor communities. People who are malnourished are more vulnerable to tuberculosis, and these are the people who face barriers accessing health services,” Dr. Adeel Tahir, senior program manager at Mercy Corps Pakistan, told Devex.
The chest camps consist of mobile vans equipped with an x-ray, a GeneXpert machine, as well as medical teams of two to three people. The program started with only three vans in 2016 and has since expanded to include 40 mobile vans equipped with digital x-ray machines. Twenty of these vans are also equipped with a GeneXpert. Together, these 40 vans run in clusters and cover 91 districts.
Previously, the Mercy Corps staff used to transport sputum samples back and forth between villages and the lab, but adding a GeneXpert machine to the vans has allowed for on-the-spot diagnosis. “By the end of the summer we hope all of the mobile vans will be equipped with GeneXpert machines,” said Tahir.




In Pakistan, Mercy Corps is bringing testing closer to marginalized communities through mobile clinics known as chest camps. Photo: Mercy Corps
In Pakistan, Mercy Corps is bringing testing closer to marginalized communities through mobile clinics known as chest camps. Photo: Mercy Corps

A chest camp in Khairpur district, Pakistan. Photo: Mercy Corps
A chest camp in Khairpur district, Pakistan. Photo: Mercy Corps

During the camps, patients first undergo symptomatic screening followed by chest x-rays. Photo: Mercy Corps
During the camps, patients first undergo symptomatic screening followed by chest x-rays. Photo: Mercy Corps
During the camps, patients first undergo symptomatic screening followed by chest x-rays. Based on these findings, the doctor in the chest camp orders sputum sample collection and a diagnostic test is run through GeneXpert, he explained. The machine can also tell a doctor if someone is suffering from drug-resistant TB to ensure they are prescribed the right treatment. “This is really helpful because if we wait for that particular patient who is suffering from drug-resistant TB to visit the TB clinic, then the chances of their survival decrease,” he said.
Because of poor health-seeking behavior in the communities and the stigma associated with the disease, it’s not enough to simply create health services.
“We have to move to certain communities where access is an issue, particularly the communities who are in far-flung areas in each district and who are marginalized because of their social status,” he said. Mercy Corps also engages respected individuals in each hotspot area ahead of each camp to help raise awareness around chest diseases, especially TB.
Dr. Adeel Tahir, senior program manager at Mercy Corps Pakistan, shares how chest camps are bringing TB testing closer to marginalized communities.
The workload on the staff has also decreased with decentralized testing. With each of the 40 mobile vans covering a cluster of two to three districts, they are able to continuously move and follow up with patients. This allows them to organize up to 20 chest camps per month.
During the first six months of 2023, they diagnosed more than 7,000 TB patients through this type of active case-finding and the treatment success rate stands at an impressive 93%, he explained.
But designing an effective and equitable TB program or intervention can’t be a top-down exercise. “Engaging communities is the most crucial step. Once you design or propose an intervention, go into the community, have a focus group discussion, invite them, tell them that this is the idea, refine it, and then implement it,” Tahir said.
More funding needed for testing in Vietnam

In recent years, Vietnam has made great strides in the fight against TB. Prevalence has declined by over 35% since 2007 while mortality dropped by 41% between 2015 to 2020, thanks to the use of innovative tools and technology, including rapid molecular testing and portable chest x-ray machines. The country is now focused on expanding access to these innovations in hotspot areas, including remote provinces.
However, one of the biggest challenges with decentralized testing is limited funding, Dr. Dinh Van Luong, the head of the executive board of the National TB Program, told Devex.
“Most funding for TB work comes from external sources that remain inadequate to meet the needs for machines and equipment, rapid diagnostic lab tests, and the training and technical transfer,” he told Devex. In addition, limited human resources and training at the lower levels of the health system also constitute barriers to deploying these new technologies.
Rapid molecular testing is easily deployed at all levels of the health care system, from primary to central laboratories, explained Luong. But while Vietnam currently counts on 332 GeneXpert machines at 179 sites, the country’s TB burden requires at least one machine in each of the country’s 700 districts, he added.
TB prevention and control systems need to be integrated within the general health system and TB care and services should be widely covered at all levels of the health system to ensure easy access to testing, diagnosis, and treatment “so that patients can be diagnosed early and put into treatments quickly, cutting off the source of infection in the community,” he said.
Advancing the global fight against TB
The social determinants of TB are likely to worsen as the war in Ukraine and the impacts of climate change continue to put a strain on everything from food and energy security to the global economy.
Many TB advocates and health care workers such as Tahir and Erau are hoping that more attention and resources will be put behind the TB response, and especially the roll out of rapid diagnostics at the primary health care level.
Without active case-finding amongst vulnerable communities and improved access to diagnostics, many TB patients’ risk delaying their treatment, or worst case, never being treated at all.
SPONSORED BY

